When someone you love is sick, you want to do everything you can for him. And for six years, I have done everything possible to make life more comfortable for my husband Steve, who has a permanent feeding tube in his stomach as a complication of heart surgery. His meals are from a can of liquid nutrition. He uses oxygen at night through a nasal cannula and occasionally during the day. In a flash, six years ago, our life together had completely changed and I earned the right to the title caregiver.
“Come with us please,” Steve wrote. How can a loving wife deny that request?
During the pandemic, Steve and I had tried to stay safe—seeing no one, repeating the mantra, “Just don’t get sick,” as if that could ward away coronavirus infection. But earlier this year, we found ourselves in the back of an ambulance heading from New York City to New Jersey, facing a new medical emergency. It was nighttime, and I was exhausted. I was hesitant to make the trip, because I was told I wouldn’t even be able to accompany Steve into the medical facility because of COVID. But Steve, unable to speak, had written a note in a small notebook he kept near: “Come with us please.” How can a loving wife deny that request?
But as the ambulance made its way through New York City traffic toward the tunnel that would take us under the Hudson River, I felt something rising in my body, something that if it could take the form of a word, would be “Enough.”
Read More: Are You the Custodial Child? The Emotional Fallout of Being Your Parent’s Caretaker
The Change
Six years ago, I first learned about intubation, feeding tubes, and what it means when your loved one has a chronic illness. My husband had an aortic valve replacement—a very serious surgery that is only given when a person’s life is in jeopardy. We had just returned from a vacation on the Amalfi Coast in Italy celebrating Steven’s 65th birthday when his cardiac doctor said, “It’s time for the surgery.”
The surgery was successful, but he developed complications that resulted in his not being able to eat solid food any longer. Our life together was completely changed. We called it the “new normal.” Italy was the last vacation we ever took together. The last plane ride, the last time we shared a meal out together, and hiking up and down the countless steps admiring the spectacular ocean was the last time we walked hand in hand outside a hundred miles of our home.
Now in 2021, the health emergency started with a minor surgery. Right before being discharged from the hospital, a nurse accidentally broke his feeding tube and replaced it with a different one since the tube Steve regularly used was on backorder. It wasn’t until we arrived home, and Steve tried to put his medications into the tube that he discovered it didn’t work. Everything he put in came gushing out. We were able to get some of it down, enough that we stopped panicking and went to sleep.
During COVID it’s been nearly impossible to get in touch with doctors and contacting Steve’s gastroenterologist was no exception. Three days later, severely dehydrated, Steve was so weak that he used the walker—kept in our closet for times like this—to see his doctor and have his feeding tube changed.
“He needs hydration,” the doctor said, but the only facility available was the emergency room. Not a great place in the best of times and much worse during COVID. I wasn’t permitted in and we communicated via texts. “Get me out of here,” he typed in all caps.
My heart dropped. My hand was shaking. I knew he needed hydration. “The beds are lined up wall-to wall. Get me out of here,” he repeated.
Right Decisions?
As a caregiver, you’re not always sure if you are making the right decision for your loved one. Steve needed to be admitted to the hospital and get hydration for a few days. We had done that in the past. But we weren’t thinking clearly. It was crisis time. It was panic mode. And so I picked him up outside the ER while he promised to hydrate himself at home.
At home, even though he had the correct feeding tube, after being dehydrated for days, he started coughing and then threw up. Throwing up for a person with swallowing problems is very dangerous. Throwing up leads to aspirating. Aspirating can lead to pneumonia.
“I’m calling 911. This is serious,” I said.
“Don’t call 911. I’m not going to the ER.”
I’ve learned over the years not to listen to my husband when he thinks he’s okay. So I dialed 911 and the medics were on their way.
“I’m sorry. I had to call,” I said.
There was no response. He was limp. His eyes were open but he wasn’t there.
“No, no,” I screamed not caring who might hear me in our apartment building. Is this how the worst happens—suddenly without preparation? My mind flew to passwords, accounts, so much I didn’t know.
Ten minutes later, the medics said, “He’s not breathing. There’s a faint pulse. We need to resuscitate.”
“Yes, yes.”
They intubated Steve right in our bedroom, lifted his body and placed him on the floor. They did whatever they had to do to get oxygen into him.
When a person is intubated, a breathing tube is inserted through the mouth and into the airway. A ventilator—also called a respirator or breathing machine—pushes air into the lungs to deliver a breath, then allows the air to come back out, just as lungs function. Intubation is the most invasive way of giving a person oxygen. It’s life support. I remember the medic’s parting words, “We’re taking him to the nearest hospital. We’re not sure he’ll make it.”
Déjà Vu and Worse
The incident was like terrible déjà vu. Exactly a year earlier, at the height of the lockdown in New York City, our beloved 15-year old cocker spaniel Cassie went into respiratory arrest in a transport to an Animal Medical Center. I was seated next to her and the memory of the attendant administering oxygen with little effect still gave me nightmares.
Like Cassie, Steve went into respiratory arrest. Unlike Cassie, the medics were able to save him and after a month at a leading New York City hospital, treated for three types of bacterial pneumonia, he was approaching the next step in his recovery.
It’s exhausting—the worrying, trying to get updates from busy doctors and nurses, my lack of sleep.
After his hospital stay, Steve was now ready to be moved to what they call a Long Term Acute Care Hospital, whose focus is weening a person off of a breathing machine.
You would think when Steve is in the hospital or a facility it’s a time for me to relax. It isn’t. I have to force myself to take a day off from visiting even if visiting is watching him sleep for two hours while I hold his hand or sit in one of the chairs in his room reading emails. Hospital staff need to know that I’m his advocate and I’m there watching.
It’s exhausting—the worrying, trying to get updates from busy doctors and nurses, my lack of sleep. But I try my very best to eat three meals a day, limit alcohol to one glass of wine with dinner, stay connected with friends and family through texts, and take long walks alone and sometimes with a friend, socially distanced. There’s a folder on my desk addressed to my niece with all of our pertinent information and final wishes just in case something happens to me.
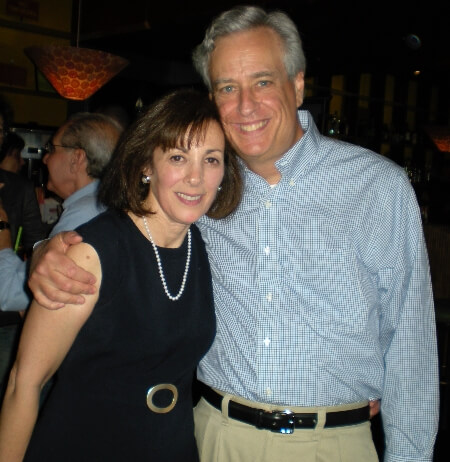
My brother promises to come visit. He lives in Florida and is waiting for his second shot. I’m making plans to get a puppy. I’m writing. It all helps while my heart is breaking. Steve and I have been married for 45-years. He’s my everything. I love him more than I ever thought possible.
Caregiver Burnout is Real
I didn’t realize it at the time, but caregiver burnout is a recognized medical condition. The Cleveland Clinic website describes it as, “a state of physical, emotional and mental exhaustion….Burnout can occur when caregivers don’t get the help they need, or if they try to do more than they are able, physically or financially. Many caregivers also feel guilty if they spend time on themselves rather than on their ill or elderly loved ones.”
Who was watching out for me?
In the transport to New Jersey, as we were getting nearer to the tunnel, I realized the temperature outside was dropping. My plan was to take an Uber back to the apartment once the transit arrived at the facility. Thoughts rushed through my mind. What if I had to wait in the cold and dark for an Uber? I had no idea where the facility was and whether there would be someplace inside where I could wait. I was concerned for my own safety.
Steve, asleep on a stretcher across from me, was hooked up to a portable breathing machine and monitored by one of the medics regularly for his vitals as the other medic drove. They were both well trained and attentive. Who was watching out for me?
Then I heard a voice barely audible say, “Let me off before you go through the tunnel.” It was a sound coming out of my body and took a few seconds for me to realize it was my voice protecting me. It was me taking care of me. I repeated the words, louder, owning them this time.
“Are you sure?” one of the medics asked.
“I’m sure.”
As the medics pulled over to the curb a few blocks from the entrance to the tunnel, I reached over and held Steve’s hand. “See you tomorrow. You’re safe. I love you but I have to take care of myself.” Without looking back, with tears streaming down my face, I left.
Read More: Help! Siblings Won’t Lend a Hand With Our Mentally Disabled Sister
***
Ann Gorewitz lives with her husband Steve in New York City. She is currently working on a memoir, “Dog Therapy: Loving and Losing Cassie” about the healing effect of loving a dog and the much needed comfort and support her beloved cocker spaniel gave her during Steve’s illnesses.





















0 Comments